Type 2 diabetes is a chronic condition that affects the body’s ability to regulate blood glucose levels effectively.
Managing this condition involves a multifaceted approach tailored to the individual’s needs,
focusing on lifestyle changes, medical treatments, and ongoing support.
This article is designed to help you better understand the impact of excess weight and its role in type 2
diabetes.
Excess weight, obesity, and morbid obesity are all risk factors for developing type 2 diabetes. Often times, individuals are not aware of the health risk of excess weight until they are diagnosed with pre-diabetes or type 2 diabetes.
What is type 2 diabetes?
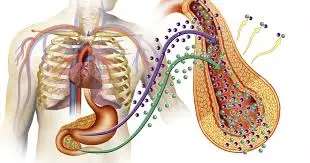
Type 2 diabetes is a chronic, potentially debilitating and often fatal medical condition requiring regular monitoring of an individual's blood sugar level and treatment. In type 2 diabetes, the body either does not properly produce or use insulin, a hormone produced by the pancreas that helps move sugar into cells. Therefore, the body becomes resistant to insulin. This resistance causes high blood sugar levels.
What are the complications of high blood sugar levels?
Excess sugar in the blood causes many health-related problems. The cells cannot get enough of the sugar they need, and when sugar levels in the blood become too high, it causes damage to nerves and blood vessels, usually in the heart, feet, hands, kidneys, and eyes.
Other complications of high sugar and insulin resistance include:
1. Increased risk of heart disease and stroke
2. Neuropathy (nerve damage, especially in extremities)
3. Nephropathy (renal impairment, kidney failure)
4. Retinopathy (vision problems, blindness)
5. Cardiovascular disease (heart disease and increased risk of stroke)
6. Erectile dysfunction in men and decreased sexual desire in both men and women
7. Depression
8. Amputation
There are a variety of blood tests that may indicate whether you have type 2 diabetes. Let's take a look at each test and see what different results could mean for you and your health.
Blood sugar level chart
The amount of sugar in your blood naturally fluctuates but stays within a normal range. The preferred way to test your blood sugar is after you've fasted overnight for at least eight hours. A fasting blood sugar level less than 100 milligrams of sugar per deciliter of blood is considered normal.
1. Frequent urination
2. Increased thirst
3. Unplanned weight-loss
4. Weakness and fatigue
5. Numbness or tingling in hands, legs or feet
6. Blurred vision
7. Dry, itchy skin
8. Frequent infections
9. Slow healing of cuts and bruises
If your blood sugar level measures from 100 to 125, you have impaired fasting glucose, and this may be an indication that you have pre-diabetes. If your blood sugar level is above 200 mg/dL, with symptoms of diabetes (see below), a second test may not be necessary to reach the diagnosis.
This test is done without any special preparation, such as fasting overnight. Even if you've recently eaten and your blood sugar level is at its peak, the level shouldn't be above 200 mg/dL. If it is and you also have symptoms of type 2 diabetes, you can expect a diagnosis of type 2 diabetes.
This test requires you to visit a lab or a healthcare professional after at least an eight-hour fast. At the office or lab, you will drink about eight ounces of a sweet liquid that contains a lot of sugar (about 75 grams). Your blood sugar level will be measured before you drink the liquid, then after one hour and again after two hours. If your blood sugar level is 200 mg/dL or above after two hours, you may have diabetes.
Losing weight is one of the most beneficial ways you can help prevent type 2 diabetes. Moderate and sustained weight loss (5 percent to 10 percent of body weight) can improve insulin action and decrease fasting sugar concentrations. For many individuals, simply adjusting their caloric intake and beginning an exercise program can greatly improve their type 2 diabetes and overall health.
Weight-loss occurs when energy expenditure exceeds energy intake. Creating a calorie deficit will result in weight-loss. Writing down the food, portion size and calorie amount in a food diary will help you become aware of the foods you consume and provide objective evidence of calorie intake.
Regular exercise helps maintain weight-loss and prevent weight regain. It also improves insulin sensitivity and glycemic control (measurement of the effects of carbohydrates on blood sugar level) and may decrease the risk of developing type 2 diabetes.
A goal should be set for 30 to 45 minutes of moderate exercise five times per week. The exercise does not need to occur in a single session to be beneficial. Dividing the activity into multiple and short episodes produces similar benefits and can enhance compliance
The Obesity Action Coalition (OAC) is the only nonprofit organization whose sole purpose is representing those affected by obesity. The OAC offers many valuable educational resources discussing excess weight, obesity, morbid obesity, type 2 diabetes and much more.
To see if you are at risk for type 2 diabetes, please schedule a visit with a healthcare professional for more information. To help you prepare for your visit, we've provided you with some great sample questions that you may be asked by a healthcare professional and sample questions for you to ask a healthcare professional.
1. Questions a healthcare professional may ask you
2. When was the last time you saw a healthcare professional?
3. When did you last have blood work completed?
4. Are you currently taking any medications?
5. Have you been previously diagnosed with any medical conditions?
6. How physically active are you on a weekly basis?
7. Can you describe your eating habits?
8. Does anyone in your family have type 2 diabetes?
9. Do you feel fatigued or tired more than usual?
10. Do you have dry-mouth or find yourself drinking fluids often?
11. Do you find yourself urinating often?
12. Do you have blurred vision or experience headaches?
13. Have you recently gained weight?
Questions for your healthcare professional
1. Do you have special training in treating diabetes?
2. Do you have special training in obesity?
3. Does your office have a registered dietitian on staff with type 2 diabetes and obesity training?
4. Do you have diabetes educators available?
5. What kind of tests do you use to determine if I have type 2 diabetes?
6. How do you prefer to treat someone with type 2 diabetes?
7. Am I at risk for any complications associated with type 2 diabetes?